As the seasons change, so does our exposure to various allergens and environmental triggers that can significantly impact our health. For many of us, this means the onset of asthma or allergies.
Understanding the nuances between these two health issues is crucial for effective symptom management. That's why at Arnot Health, we are dedicated to empowering our community with essential health information and support for a happier, higher quality of life.
We'll cover everything you need to know about allergies and asthma this year, including how to recognize symptoms, manage your condition, and seek professional treatment.
Understanding Allergies
Allergies occur when your immune system reacts to a foreign substance — such as pollen, bee venom, pet dander, or even certain foods — that doesn't cause a reaction in most people. Your immune system produces substances known as antibodies. When you have allergies, your immune system makes antibodies that identify a particular allergen as harmful, even though it isn't. When you come into contact with the allergen, your immune system's reaction can inflame your skin, sinuses, airways, or digestive system.
During allergy season (which typically peaks in the spring and fall), certain allergens are more prevalent and can be particularly troublesome. Here are some of the most common ones:
- Pollen: This is one of the most common triggers of seasonal allergies. Trees, grasses, and weeds release these tiny grains into the air to fertilize other plants. When they enter the nose of someone who is allergic, they can trigger sneezing, itching, and a runny nose.
- Mold: Mold spores float in the air like pollen, but they thrive in damp, humid areas. Outdoor molds can be found in poor drainage areas, such as in piles of rotting leaves or compost piles. Indoors, they can be found in basements or bathrooms. Mold allergies typically peak in warm, humid seasons.
- Dust Mites: These tiny creatures thrive in warm, humid environments and are a common year-round trigger. They live in bedding, upholstered furniture, and carpets. Their waste is what triggers allergic reactions, which are often worse in the winter when homes are heated and windows are closed.
Seasonal allergies can be more than just a nuisance; for many, they significantly impact respiratory health, leading to uncomfortable (and sometimes severe) breathing difficulties.
When allergens such as pollen, mold, or dust mites enter the body through inhalation, they are identified as invaders by the immune system. In response, the immune system releases chemicals like histamine, which are intended to expel these foreign particles. This chemical release leads to the inflammation of nasal passages, sinuses, and airways in the lungs; the resulting reaction is the body's attempt to block the allergen from spreading.
This inflammation can cause several respiratory symptoms, including:
- Nasal congestion and runny nose: These are common reactions as the nasal passages swell and produce extra mucus to flush out allergens.
- Sneezing: Frequent sneezing is a reflex to expel irritants from the nasal cavities.
- Itchy or watery eyes: This occurs when histamine also affects the tissues around the eye area.
- Coughing: This is a response to the irritation in the throat and airways, which can be exacerbated by postnasal drip.
- Wheezing and shortness of breath: For those with sensitive airways or pre-existing respiratory conditions, seasonal allergies can cause shortness of breath. As the airway muscles tighten, it becomes more difficult to breathe.
Asthma Explained
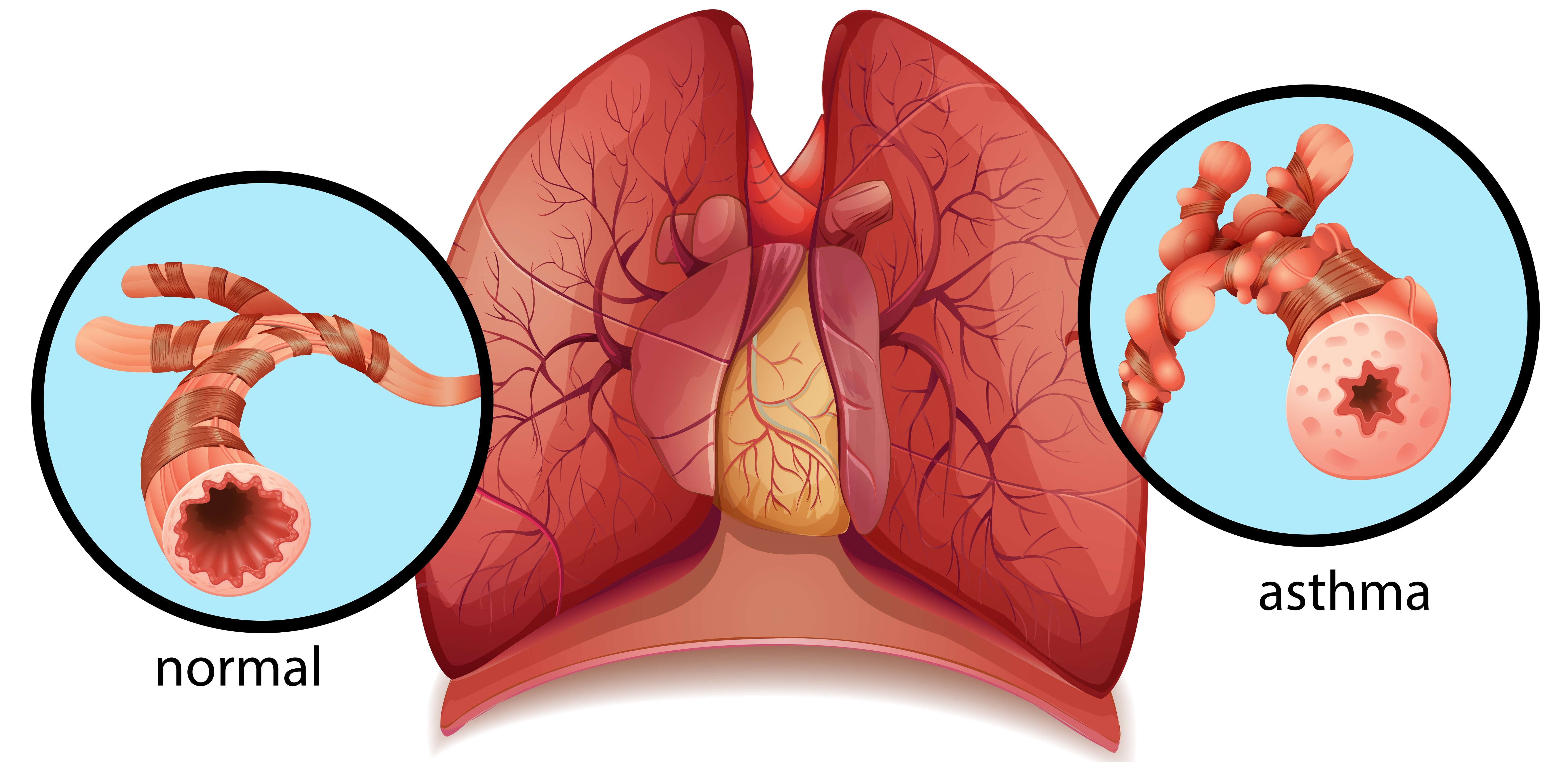
Asthma is a chronic respiratory condition that affects millions of people worldwide. It is characterized by inflammation and narrowing of the airways, which can lead to recurring periods of wheezing, shortness of breath, chest tightness, and coughing. These symptoms are often made worse by certain triggers, including allergens, cold air, exercise, or even stress.
The airways in a person with asthma are more sensitive than those in someone without. When exposed to triggers, the muscles around the airways tighten in a process known as bronchoconstriction. Simultaneously, the lining of the airways becomes inflamed and starts to swell, and the cells in the airways produce extra mucus. This mucus is thicker than normal, which further obstructs the airways.
These changes in the airways make it harder for air to flow in and out of the lungs, leading to the following symptoms of asthma:
- Wheezing: A whistling or squeaky sound that occurs during breathing, particularly when exhaling, is one of the hallmark signs of asthma.
- Shortness of breath: Individuals with asthma often feel like they can't get enough air into their lungs. This sensation can range from mild discomfort to severe distress, depending on the severity of the asthma attack.
- Chest tightness: This can feel like something is squeezing or sitting on the chest, making it difficult to breathe.
- Coughing: Particularly frequent at night or early in the morning, coughing in asthma is often a response to the irritation caused by inflammation and mucus in the airways.
Asthma Vs. Allergies: Connections and Differences
So, what's the difference between asthma and allergies? They are often grouped because they share several symptoms and can be interconnected, but they are distinct reactions. While both conditions can affect breathing, the specific symptoms vary.
Allergy symptoms are specifically triggered by allergens, mediated by histamine release. They manifest through common symptoms such as sneezing, a runny or stuffy nose, itchy or watery eyes, and skin rashes. These reactions primarily stem from the body's immune response to allergens like pollen, dust mites, or pet dander.
Asthma, on the other hand, involves a more complex response that affects the airways and breathing more directly. It primarily impacts the lower respiratory tract, leading to symptoms such as wheezing, shortness of breath, chest tightness, and coughing. These symptoms are caused by the narrowing and inflammation of the airways.
Managing Overlapping Conditions
For those with both allergies and asthma, it is important to identify and avoid triggers as much as possible. Treatment may involve a combination of antihistamines to control allergies and bronchodilators or anti-inflammatory medications to manage asthma. Additionally, immunotherapy (allergy shots) might be recommended to decrease sensitivity to allergens, potentially reducing both allergic reactions and asthma symptoms over time.
What is Allergic Asthma?
For many individuals, there is a direct link between allergies and asthma, a condition often referred to as allergic asthma. In allergic asthma, the same allergens that trigger allergy symptoms may also trigger an asthma attack. This occurs because the allergens cause inflammation in the airways, making them more sensitive and reactive to irritants.
When a person with allergic asthma inhales an allergen, their immune system responds by releasing substances that inflame the airways in addition to the typical allergic reactions. The resulting inflammation can lead to an asthma attack, characterized by severe wheezing, coughing, or difficulty breathing.
Unlike other types of asthma, allergic asthma is directly linked to an allergic reaction. While non-allergic asthma can be triggered by irritants in the air, physical activity, or cold weather, allergic asthma is triggered by allergens. This means that people with allergic asthma often experience a seasonal pattern to their symptoms, correlating with the presence of specific allergens in the environment.
Signs of Allergy Induced Asthma
It can sometimes be difficult to distinguish between regular seasonal allergies and allergic asthma, but certain symptoms will indicate when allergies have escalated:
- Wheezing and Shortness of Breath: While typical allergy symptoms include a runny nose and itchy eyes, the addition of wheezing or a persistent cough may suggest allergic asthma. Shortness of breath, especially after exposure to allergens, is a key indicator.
- Chest Tightness: Feeling a tight sensation in the chest during allergy season, particularly after exposure to allergens, can be a sign of allergic asthma.
- Difficulty Breathing After Allergen Exposure: If breathing difficulties follow shortly after exposure to known allergens, this is a strong indication of allergic asthma.
- Nighttime Symptoms: Experiencing asthma symptoms such as coughing or wheezing at night can suggest allergic asthma.
If you suspect that your seasonal allergies may have progressed to allergic asthma, it is important to consult with a healthcare provider. They can perform tests to confirm the diagnosis and recommend a treatment plan that addresses both conditions, often involving inhalers, allergy medications, and possibly allergy shots to reduce sensitivity to triggers.
Managing Asthma or Allergies During Peak Seasons

Navigating the challenges of peak allergy and asthma seasons requires a proactive approach to managing your symptoms effectively. Here are a few practical tips and strategies to keep in mind!
Tips for Managing Seasonal Allergies
Seasonal allergies can disrupt daily life, but with the right strategies, you can minimize your discomfort a great deal.
One of the most effective ways to manage allergy symptoms is to limit exposure to allergens. On days when pollen counts are high, try to stay indoors — especially during midday and afternoon hours when pollen levels are at their peak. Keeping windows closed and using air purifiers in your home may also help reduce exposure to pollen and other airborne allergens.
A variety of over-the-counter and prescription medications can also alleviate allergy symptoms. Antihistamines are commonly used to counteract the body's histamine response, which is responsible for runny noses, sneezing, and itching. Nasal sprays, including corticosteroid sprays, reduce nasal inflammation and congestion.
It's important to start these medications before symptoms begin if possible, as they can be more effective at preventing symptoms rather than treating them once they've started.
Tips for Asthmatics During Allergy Season
For asthmatics, allergy season can be particularly challenging, as allergens may trigger severe asthma symptoms. Asthmatics must adhere to their prescribed medication regimen, especially during this time of year. Regular use of inhalers (particularly corticosteroid inhalers) can help keep inflammation under control and prevent asthma attacks triggered by allergens.
Note that seasonal changes can additionally affect asthma control. If you notice an increase in asthma symptoms or if your usual medications seem less effective, it may be time to consult your doctor. Healthcare providers can assess whether adjustments to your treatment plan are needed, such as modifying dosages or adding additional treatments to help manage symptoms during high-risk times.
Breathe Easy with Arnot Health
If you're experiencing asthma or allergies, you don't have to face it alone! At Arnot Health, our specialists are here to help with personalized care plans tailored just for you. Schedule an appointment with us today and take back control of your health this season!

